Computer Chronicles Revisited 50 — The Cemax-1000, Poisindex, PUFF, and the EXPERT System
This episode of Computer Chronicles from November 1985 returned to a favorite topic of the show: artificial intelligence and expert systems. Here, the focus was on the practical applications of such technology to the field of medicine. Essentially, how could computers be used to improve the delivery of health care?
From Artificial Hearts to a “Doctor in a Box”?
To kick things off, Stewart Cheifet presented his cold open from Penn State’s Milton S. Hershey Medical Center in Hershey, Pennsylvania. He held the Penn State Heart, a mechanical artificial heart that had recently been used to keep a man named Anthony Mendia alive for 10 days. But that was nothing compared to another prototype that Cheifet displayed, a new artificial heart with a microprocessor inside that could control all of the device’s functions. Cheifet said this device would be ready for human use in about five years and was just one example of how computer technology could be used in medical research.
Back in the San Mateo studio, Cheifet showed off a Drexon Lasercard to Gary Kildall. (This was the second time Cheifet had used this prop; it previously made an appearance back in a May 1984 episode on storage devices.) It looked like a credit card but actually contained 800 pages of medical information, including X-rays, EKGs, and a patient’s complete medical and pharmaceutical history. Cheifet noted this wasn’t something out of “Star Trek,” but something being used right now by Blue Cross in Maryland. He said it was a good example of how computer technology was being used in the medical field.
Kildall noted that medicine, like law, was very information-intensive and something like the Drexon Lasercard could help manage that information. But computers had a wide variety of potential uses in medicine. Someday, he quipped, artificial intelligence and expert systems could lead to a “doctor in a box.”
Using Computer Graphics to Perfect Plastic Surgery
In her first remote segment, Wendy Woods reported on the work of Contour Medical Systems, a California company that used computer graphics to design replacement parts for the human body. Woods noted the most common tasks given to computers were time-consuming or tedious jobs that humans didn’t like to do. But in the medical field, computers were more than time-savers.
Woods said that Contour’s imaging processing computer–known as the Cemax-1000–was capable of reconstructing the shape of damaged body parts to enable “nearly flawless” repairs. Working from X-ray slices taken by a computerized tomography scanner, the Cemax could create three-dimensional images of bone structure or soft tissue. For many kinds of surgery, Woods noted, it represented a major departure in method.
Dr. David N. White, a plastic surgeon and co-founder of Contour, told Woods this work began when he was a junior resident at Stanford and saw the means by which facial reconstruction surgery was performed. You would essentially take a planar projection X-ray that would have multiple overlying shadows and try to make a diagnosis on that basis. Once you did that, White said, you would go to the operating room, open the patient, and try to reconstruct what you thought was there. But often, the surgeons found that their diagnosis in the operating room was different then what they had initially thought. The doctors would then have to take a piece of bone from elsewhere in the patient’s body and carve it to match the part needed for the reconstruction.
White said this process was more art than science, so by using the computer in this way, his goal was to make the process a more well-defined scientific exercise. Woods explained the Cemax system began by highlighting selected areas of the scanned image, picking out the boundaries of different tissue densities. Each area could then be examined to assess the kind of surgery required.
In the case of damage to one side of the face, Woods said, Cemax would first create a mirror image of the intact side and then fill in the missing parts for perfect symmetry. The software provided a neat, mathematical solution to an aesthetic problem–with some limitations. White said that computers would not replace surgeons and what one could deliver in the operating groom was affected by things other than mathematics and cybernetics.
To complete the process, Woods said, once the program had designed a screen model of the missing facial part, a software-driven milling device created a plastic mold. This yielded a precise model of the final synthetic or bone-graft replacement.
White told Woods that he expected there would be a “computer explosion in medicine” over the next few decades and this was the beginning of an exciting era where the computer and physician would be inextricably linked.
Moving Doctors from Textbooks and Microfilm to CD-ROM
The first round table segment for this episode featured Mark Tuttle of the University of California, Berkeley, and Dr. Ben Honigman of the University of Colorado Medical Center. Kildall asked Tuttle, a specialist in the use of medical technology, about the overall effectiveness of computers in medicine. Tuttle replied that in some areas computers had been “extremely effective,” and in other areas “not effective at all.” He noted that whenever a patient walked into a doctor’s office or emergency room, almost anything could be relevant to their medical problem. So at that point, computers were not terribly useful because they couldn’t be programmed to measure “relevance.” On the other hand, as the patient’s problem became more narrowly defined–i.e., eliminating the 99.9 percent of things that were not relevant–you got into more specialized knowledge, and at that point computers had been successfully applied in a number of contexts.
So the problem was in making the initial diagnosis, Kildall asked? Tuttle said yes, again because of the problem of determining relevance.
Kildall then asked Honigman, the director of the University of Colorado hospital’s emergency room, to demonstrate Poisindex, a CD-ROM database used by doctors to help diagnose toxicology cases. Honigman said the database also contained information about a number of different areas, including drug and clinical information. Honigman said Poisindex was used not just in the ER but also by critical care and intensive care doctors.
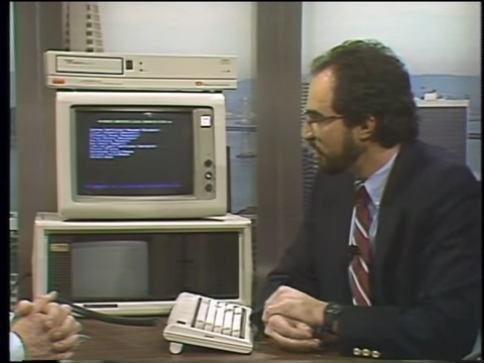
Honigman used the software–running on a Compaq Portable hooked up to a CD-ROM (see image below)–to illustrate a sample toxicology case. In this example, a child was found next to a bottle of aspirin. Poisindex contained information about aspirin from different manufacturers and what each of their respective pills contained. Kildall clarified that Poisindex was a purely local database that did not require online access. Honigman said yes, everything was stored on 250 MB CD-ROM discs.
Honigman continued his hypothetical example, showing how Poisindex could provide information regarding the proper treatment for the patient. Tuttle interjected, asking whether a doctor wouldn’t already know the treatment for something like aspirin toxicity. Honigman said there were some idiosyncrasies about the treatment in terms of severity. A mild toxicity case called for different kinds of therapy that severe toxicity. By inputting laboratory blood test results, the software could assess that severity, he added.
Kildall asked how doctors would have found this type of information before something like Poisindex. Honigman said you’d need to manually search textbooks, journals, and microfilm. Tuttle added the doctor might also have made the wrong diagnosis. Honigman said the benefit of Poisindex was that once a diagnosis was made, the information could be printed off in the emergency room and handed off to another department. The software could also print out the specific dosages of medication required for a child based on their age and estimated weight.
Kildall asked if doctors ran the risk of being sued for malpractice if the information in Poisindex was wrong. Honigman said it was a gray area as far as the courts were concerned. Nobody had an answer yet. He thought that just as medical textbooks were historically deemed appropriate sources of information, so too were computers.
Cheifet noted that doctors seemed to be slower in adopting computers than lawyers or business professionals. He asked Tuttle why that was. Tuttle said one issue was the fundamental confusion about the worth of the doctor’s judgment. Some medical professionals took pride in making a diagnosis from memory, while no mathematician or engineer would design a bridge and say, “I’m giving my client more of their money’s worth because I designed it in my head rather than using formulas.” Honigman added that another issue was that until recently, computers had not been very user-friendly. It was easier just to look up information in a book.
Duplicating a Doctor’s Experience in Software
Wendy Woods presented her second remote segment, this time from Pacific Presbyterian Medical Center in San Francisco (now known as California Pacific Medical Center), where she discussed PUFF, an artificial intelligence system used to diagnose lung disease. Dr. Robert J. Fallat designed PUFF in conjunction with Stanford University. Woods said the system duplicated Fallat’s own thought processes. It assimilated data from patient tests and translated it into athe diagnosis that Fallat would make himself. Michael Kerrins, a staff member at Presbyterian Hospital, said PUFF spoke the same way that Fallat spoke, even using his punctuation.
Woods said that PUFF ran on a Tektronix terminal connected to a hard disk drive. Its central memory bank was currently being revised for the first time in four years. If the new version proved successful, PUFF would take on the name MicroPUFF and work on personal computers. And it would be commercially available from Medical Graphics, a company based in St. Paul, Minnesota.
Woods said the biggest selling point for this type of software was the time savings. Kerrins said that time savings was “phenomenal.” Presbyterian had been able to increase its patient load by 100 percent using PUFF over the past two years, he said, without having to increase its staff.
Woods noted that medical costs were currently rising at three-to-four times the national inflation rate. But that wasn’t the case at Presbyterian’s pulmonary lab thanks to PUFF. When you hired a computer instead of people, she quipped, you saved money.
Using Computers to Help Front-line Medical Personnel in Developing Countries
For the second and final round table, Dr. Chandler R. Dawson and Dr. Mark Musen joined Cheifet and Kildall. Kildall commented to Musen, a doctor who specialized in computers and medicine at Stanford University, that when he was in school 10 years earlier there was always some AI project going on related to medical diagnosis. Had there been any progress on that front in the last 10 years? Musen said there had been “enormous” progress. He noted that much of the research in artificial intelligence had been directed at the medical field. He added that the work completed over the past decade was now starting to be put into practical use.
Kildall asked Musen about his own expert system project. Musen said it was called ONCOCIN, which provided advice to doctors taking care of chemotherapy patients. Kildall asked if this was being used on actual patients. Musen said it was being used in an experimental trial at Stanford’s oncology clinic.
Kildall asked if the doctors liked the system. Musen said doctors approached using computers and software like ONCOCIN with “some degree of ambivalence,” although they were surprised at how well it gave advice in certain contexts. When expert faculty members reviewed cases where the treating physician’s diagnosis differed from the computer, the expert sided with the computer about half the time and the doctor half the time.
Cheifet asked for a specific example of how ONCOCIN was used. Musen explained the system was used with patients undergoing intensive cancer treatments. Generally that involved many kinds of drugs given in a specific sequence over time. ONCOCIN determined the appropriate treatment based on the patient’s laboratory tests and how they were responding to previous treatments. ONCOCIN could also advise when further laboratory testing were necessary.
Kildall turned to Dawson, an ophthalmologist and director of the Proctor Foundation at the University of California San Francisco, to demonstrate his own expert system, which ran off a PC. (They don’t name this software on-air but it was just called the EXPERT System and originally developed at Rutgers University.) Dawson said his system was developed to diagnose people with eye problems. But it was aimed at health care delivery in developing countries to help front-line workers with very little training.
Dawson then provided a demonstration of his system software running on a normal PC. Kildall mentioned his 14-year-old daughter had an eye infection, so they decided to use her as their hypothetical case. (I’m not going to walk through the specifics here.) Essentially, the expert system asked a series of questions about the patient’s symptoms. Dawson explained that the program did not actually make a diagnosis. The doctor still had to enter a presumptive diagnosis and treatment based on the information provided. The software could then advise local health care personnel on what specific actions to take, such as administering topical antibiotics, based on their available resources.
Kildall said this type of software would be appropriate for use with a hand-held computer. Dawson said that was the goal, to use small portable machines with erasable programmable memory (EPROMs). But ideally they could use something like CD-ROM technology as that would allow the system to show pictures to illustrate various medical conditions.
Cheifet asked if this technology could eventually be adapted for home computers in the United States. Dawson said that would be a potential goal, particularly for helping people to sort out problems that were serious from those that were not as serious.
Kildall asked how close Dawson’s system was to being a completed product. Dawson said it was still in a “beta testing” phase. The plan was to conduct field tests of the system in north Africa during the winter of 1986.
Kildall asked both guests if they actually saw expert systems like these replacing the traditional medical diagnosis process over the next 10 years or so. Musen said that was a difficult question because most of the current work was still experimental. He said there were still a lot of fundamental questions in artificial intelligence that needed to be solved before we would see many practical expert systems.
Cheifet asked Dawson if computer training was getting into medical schools. Were doctors learning about this type of technology? Dawson said it was being introduced more and more at the medical school level. At the postgraduate level in particular doctors were using computers to access the National Library of Medicine database to lookup specific subjects quickly.
Why Computers and Doctors Were a Natural Match
In his closing commentary, George Morrow said computers and medicine went well together. He said there were three reasons for this. First, computers were now a part of a doctor’s life from the time they started school until well into their practices. Second, medicine by its nature was filled with “disappointments and failures,” and any device that reduced that offered powerful psychological feedback for the doctor. Third, doctors were trained to be suspicious of data, whether it was from an experiment or the symptoms of a patient. When doctors applied this same suspicion to computers, they made sure that the software was well tested.
Motorola Proposed Wireless Computer Networking While Mitsubishi Debuted First Picturephone
The Internet Archive’s record of this episode is actually a rerun from May 1986, so that’s when this “Random Access” segment by Stewart Cheifet originally aired.
- Apple president John Sculley told industry analysts that the company would soon offer MS-DOS as an option on the Macintosh. Apple would not get into the PC clone business, Sculley said, but both MS-DOS and UNIX would be available on future Mac systems.
- Sperry and Burroughs were in merger talks. The combined firm would have annual computer sales of over $10 billion, Cheifet noted, making it second only to IBM. Both companies’ stock prices had soared, indicating strong support for the deal.
- The British Library had been looking to convert to optical storage. But after testing CD-ROM, Cheifet said the British were challenging claims that laser disc storage would “last forever.” The Library said its research found that within 10 years, the coating on the discs would crack, leading to oxidation of the underlying aluminum surface. While such cracks would not affect audio or data, it would be “catastrophic” for archival storage of data.
- The Federal Communications Commission requested comments on a proposal by Motorola to create a “wireless computer network.” Motorola wanted to connect local computers and peripherals up to 500 feet using low-powered radio frequencies.
- The House Judiciary Committee sent a computer crime bill to the floor.
- Paul Schindler reviewed An Apple a Day (Avant Garde Publishing Corporation, $79.95), a program to help users keep their medical records and emergency contact information on a floppy disk. It also included an online medical encyclopedia. Schindler said the program was a great idea but “tedious to look at” given the lack of color.
- Toshiba released the first AT-compatible laptop, which featured a full-size gas plasma display, a 1O MB hard drive, and a 3.5-inch floppy disk drive. Data General also announced its second-generation laptop, the DG-2, which had an electroluminescent display, 10 MB hard disk, and up to 640 KB of RAM.
- The June 1986 Sharper Image catalog would feature the world’s first “picturephone.” The technology had been around for 20 years but never quite taken off, Cheifet said. But Mitsubishi was now releasing a home picturephone priced at under $1,500. It sent still photos over ordinary phone lines, but you couldn’t talk while the system transmitted the pictures.
- Carnegie Mellon University had a new project called Sexpert, a sex therapy program developed by Dr. David Servan-Screiber. Cheifet said the program asked couples approximately 100 multiple-choice questions and recommended a treatment program.
Medical Expertise in BASIC?
Medical technology is a difficult field for a layperson like myself to research and comprehend. So I won’t delve much into the various products demonstrated in this episode. But I do have a couple of comments. The first is that many developers of these early medical expert systems used BASIC to convert their software from minicomputers–which was usually written in something like LISP–to PCs. This was done with both PUFF and and Dr. Dawson’s EXPERT system. Indeed, Dawson and several colleagues wrote in a 1984 paper for the Journal of Medical Systems that they translated their original software model, which was built on a DEC-20, to BASIC code that could run on an IBM PC, Apple IIe, or Epson HX-20 hand-held computer.
My second note relates to the Cemax-1000. Although discussed here purely in the context of medical imaging for use in surgical reconstruction, this was in fact an early 3-D graphics computer. Contemporary reporting talked about the Cemax as a competitor to the Pixar Image Computer and the Silicon Graphics IRIS workstations. For example, in a 1987 article for Computer Pictures, Abigail Christopher said that Pixar’s machine was actually being used in beta testing to not only design artificial limbs and joints but also help doctors rehearse procedures, something the Cemax could not do.
Notes from the Random Access File
- This episode is available at the Internet Archive and had an original broadcast date of November 12, 1985, although as previously noted the episode I reviewed was a rerun that aired on May 9, 1986.
- Anthony Mandia, the artificial heart patient referenced by Stewart Cheifet in his opening, suffered from cardiomegaly, i.e., an enlarged heart. According to an account of Mandia’s case published by Penn State in October 1985, Mandia’s heart was twice the normal size of a healthy heart and was in congestive failure. On October 17, 1985, doctors realized Mandia’s condition was critical, and lacking an available donor heart, Penn State cardiologist Dr. Dwight Davis recommended implanting the artificial heart. The procedure took about four hours. The artificial heart was only meant to be temporary until a donor heart could be found. Sadly, it never was, and Mandia died due to “organ system failure secondary to overwhelming infection,” according to the Associated Press. Mandia was 44. United Press International added that 11 people, including Mandia, had received an artificial heart up to that point, and only five were still living.
- Dr. Chandler R. Dawson died in March 2013, according to a short obituary published in Princeton University’s alumni newsletter. Dawson received his medical degree from Princeton in 1952 and served as director of the Francis I. Proctor Foundation at the University of California San Francisco from 1984 until 1995. The Proctor Foundation focuses on the study of trachoma–an infection that causes blindness–and other eye diseases.
- Dr. David White’s Contour Medical Systems later changed its name to Cemax, Inc., reflecting the name of the company’s main product. Cemax merged with ICON Medical Systems in 1995 to form Cemax-Icon, Inc. In 1997, Imation Corporation acquired Cemax-Icon in a cash-and-stock deal valued at $79 million. A year later, in December 1998, Imation sold Cemax-Icon to the Eastman Kodak Company. Kodak, in turn, consolidated Cemax-ICON into its preexisting medical imaging business. As for Dr. White, he’s still licensed and presumably practicing as a plastic surgeon in Claifornia.
- Dr. Benjamin Honigman spent 33 years at the University of Colorado School of Medicine and retired in 2018. Honigman’s work in emergency medicine focused on the impact of high altitudes on the human body and he served as director of the hospital’s Altitude Medicine Clinic from 2003 to 2014.
- Dr. Mark Musen is still with Stanford University after nearly 40 years, having started as an internal medicine fellow back in 1983 and serving as director of the Stanford Center for Biomedical Informatics Research since 1993.
- As far as I know, Apple never released any MS-DOS or UNIX-compatible Macs during John Sculley’s tenure. It was possible to emulate DOS functionality on many early Macs using software, as illustrated by this 1992 Apple brochure. But the only example of a DOS-compatible Mac that I’m aware of was the Power Macintosh 6100/66 released in 1995. (Credit to Clint Basinger of LGR for that information.)
- The merger of Burroughs and Sperry went through to form Unisys Corporation, which still exists today.
- The FCC received a bunch of comments but never took any formal action on Motorola’s wireless networking proposal. This was not the precursor of modern wi-fi, which is based on the IEEE 802.11 standard developed in the 1990s.
- If Paul Schindler was lukewarm about An Apple a Day, Cynthia E. Field of InfoWorld was positively hostile. Her review dismissed the program as “unpolished” and filed with information that was “trite and useless in emergencies.” She noted the software included multiple “printed disclaimers of any responsibility by the publisher for the reliability and accuracy of the program’s information.” This prompted a defensive letter to the editor from Avant Garde president Tom Measday, who said the disclaimers “were not our choice but a requirement of our attorneys.” The editors fired back, “While lawyers may demand that publishers absolve themselves from responsibility for information provided by software, buyers are less likely to do so.”
- That Toshiba AT-compatible laptop was known as the Toshiba T3100. It originally retailed for $4,495. The Data General laptop would actually be called the Data General/One Model 2 and retail for $4,635.
- The Mitsubishi picture phone was known as the Lumaphone (or Luma LU-1000) and it actually began as a project at Atari, Inc. Atari had established a division called Ataritel back in 1981 to work on telecommunications projects, including a videophone. After the sale of Atari’s home video game and computer assets to Jack Tramiel in July 1984, Warner Communications retained Ataritel for a short time before selling that division as well to Mitsubishi.